Lupus: Symptoms, Diagnosis, and Disease Management is a thorough guide to understanding this chronic autoimmune disease. Imagine experiencing a mysterious illness, with symptoms that vary and mimic other conditions. This is the reality for many people diagnosed with lupus. This guide will walk you through the essential facets of lupus, from recognizing the symptoms and navigating the diagnostic process to understanding effective disease management strategies. We’ll explore the key factors in accurately diagnosing lupus, the spectrum of potential symptoms, and discuss various treatment options, to empower you with knowledge and a proactive approach to managing this challenging condition. This article will be divided into sections covering symptoms, diagnosis methods, treatment approaches, and available resources for support.
Understanding the Spectrum of Lupus Symptoms
Recognizing the Diverse Presentation of Symptoms
Lupus is notoriously complex due to its diverse scope of symptoms, which can vary greatly from person to person and even change over time. This heterogeneity in symptom presentation makes early diagnosis challenging. Common symptoms include fatigue, joint pain and swelling, skin rashes, and fever, however, these are just some of the possible symptoms that can present variedly for every individual. A notable symptom is the butterfly rash, which often manifests across the bridge of the nose and cheeks, however, other forms of skin rashes can present in many forms and are also difficult to distinguish. Additionally, individuals with lupus might experience a variety of other symptoms such as inflammation and swelling in the joints or organs. This can also include cardiac issues, kidney problems, or neurological symptoms. The lack of easily identifiable markers, coupled with these often overlapping symptoms, is a significant challenge in recognizing lupus. Many patients often report experiencing a wide scope of flu-like symptoms or chronic pain before receiving an accurate diagnosis. This often outcomes in a longer diagnostic process, causing significant distress and confusion for patients and their families.
Diagnostic Approaches for Lupus
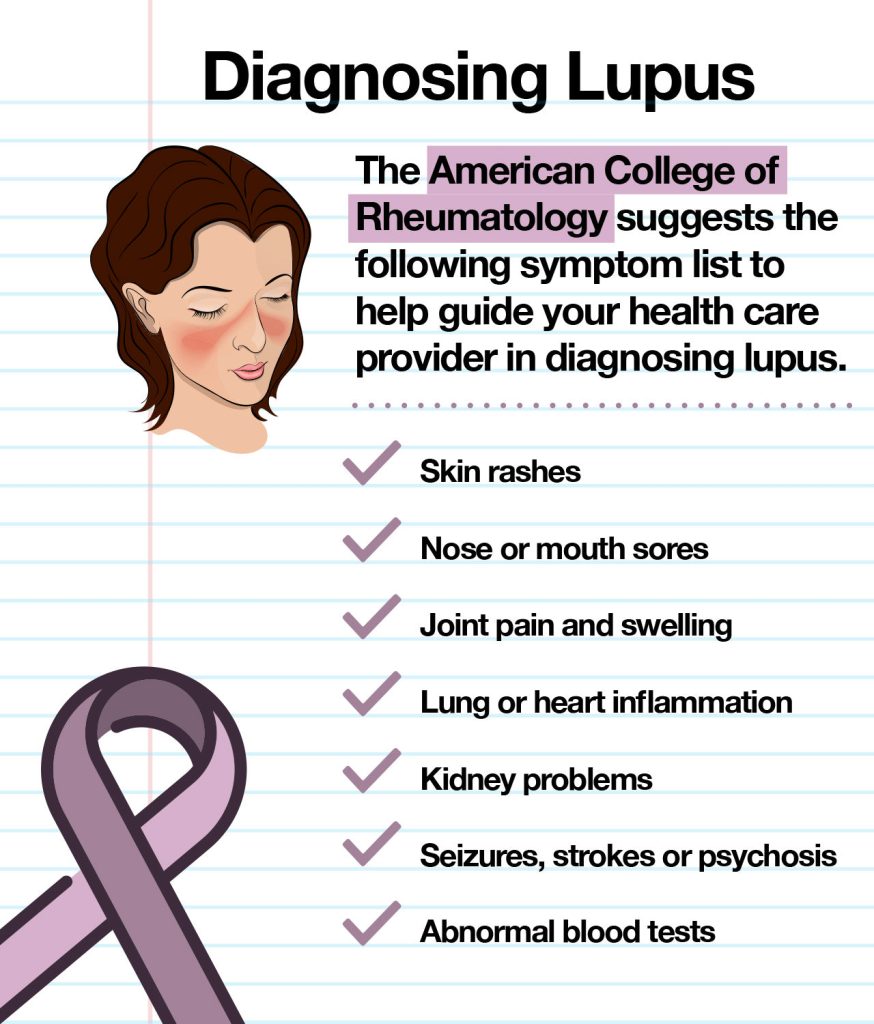
The Multifaceted Process of Diagnosing Lupus
Diagnosing lupus requires a multifaceted approach, as there’s no single test to confirm the diagnosis. Instead, healthcare offerrs rely on a combination of clinical evaluation, blood tests, and sometimes, even biopsies. Clinical evaluation includes careful examination of the patient’s medical history, family history, and physical examination findings. Blood tests are essential, often revealing markers of inflammation and antibodies associated with lupus. For instance, antinuclear antibodies (ANAs) are commonly present in lupus, however, it’s critical to remember that ANAs can also be found in other autoimmune conditions. These antibodies play a function in recognizing the presence of abnormalities in the body’s immune system that are associated with lupus. The diagnostic process often involves a series of tests to exclude other conditions with overlapping symptoms. This thorough approach ensures that the diagnosis is accurate and appropriate for the patient’s specific situation.
Managing Lupus: A Holistic Approach
Personalized Strategies for Effective Management
Effective lupus management is a personalized journey, with no one-size-fits-all solution. It relies heavily on a collaborative approach between the patient and their healthcare team, including rheumatologists, primary care physicians, and other specialists. One key facet is managing symptoms effectively. Pain management strategies, including over-the-counter medications and more targeted treatments, may be necessary to alleviate chronic pain and discomfort. Moreover, regular exercise, stress management techniques, and a balanced diet can significantly impact overall well-being and reduce flare-ups. A critical component of lupus management is medication adherence. Monitoring medication efficacy is crucial and any adverse reactions must be reported immediately to the medical team. Furthermore, ongoing monitoring of organ function and potential complications is essential in maintaining the patient’s long-term health. In many cases, patients are advised to regularly visit their specialists for checkups and blood work.
Lupus and its potential impact on well-being
A thorough Understanding of the Disease
Living with Lupus can significantly impact a patient’s physical and mental well-being. Chronic fatigue and pain can lead to reduced productivity and participation in daily activities. This can affect social relationships and overall quality of life. Psychological well-being is just as crucial as physical health; therefore, it is equally critical to support patients experiencing psychological stress. Mental health resources should be readily available, which may include therapy or support groups.
Lupus Resources and Support Systems
Finding the Right Support and Information
Several resources and support systems can aid individuals living with lupus. These can offer access to information, emotional support, and practical advice. Support groups can offer a safe space for sharing experiences and connecting with others facing similar challenges. Furthermore, online communities and forums can offer valuable resources for information sharing and peer-to-peer support. Many healthcare offerrs offer access to additional lupus resources and support systems as well.
How prevalent is lupus in the general population?
The prevalence of lupus is estimated to affect 1.5 million Americans alone. The prevalence differs based on ethnicity, gender, and geographic location. This means that the prevalence might change significantly based on the specific group of people being observed.
What are the long-term implications of lupus?
Lupus can have various long-term implications, including the potential for organ damage. The impact on daily living and mental health is equally crucial to consider. It can impact work, social relationships, and overall well-being. Therefore, management and support are crucial to improving long-term well-being. Early intervention with support systems and management is critical for mitigating the effects of long-term lupus.
What treatments are available for Lupus?
Current lupus treatments primarily focus on managing symptoms and slowing disease progression. Treatment plans are tailored to each individual and may involve various medications, including corticosteroids, immunosuppressants, and antimalarials. The achievement of treatment can vary from person to person. Understanding the individual response to varied medications and treatment approaches is crucial to optimal treatment efficacy.
Can lupus be cured?
Currently, there is no cure for lupus. However, with proper management and adherence to a treatment plan, individuals can effectively control the disease and live fulfilling lives. Managing symptoms through a collaborative approach with healthcare professionals is a crucial factor to improve the overall quality of life and minimize potential complications. Continuous monitoring and adherence to the prescribed treatment plan is critical to improve outcomes. Early intervention and understanding the disease’s complexity are equally crucial factors that can positively influence patient outcomes and quality of life.
Frequently Asked querys
What are the common diagnostic symptoms of lupus?
Common diagnostic symptoms of lupus include fatigue, joint pain, skin rashes, and fever. These symptoms, however, can vary widely from person to person. The absence of one particular symptom should not lead to a dismissal of lupus as a possible diagnosis. The diagnostic process is multifaceted, involving a combination of clinical evaluation, blood tests, and other analyses to determine patterns and rule out other potential conditions.
In conclusion, Lupus: Symptoms, Diagnosis, and Disease Management presents a complex medical challenge requiring a multi-faceted approach. Understanding the various symptoms, diagnostic processes, and available management strategies is crucial for both patients and healthcare professionals. Early diagnosis and proactive disease management are paramount to improving patient outcomes. Seeking a specialist’s guidance is recommended for effective long-term management and support. Are you looking for more personalized guidance on managing your lupus? Schedule a consultation with a rheumatologist today!